 Dr. Prithvi Mohandas
Dr. Prithvi Mohandas
Managing Director of MIOT International and
Secretary, IGOF
A review of minimally invasive hip replacement surgery – current practice and the way forward
N.A. Siddiqui, P. Mohandas, S. Muirhead-Allwood, T. Nuthall
The London Hip Unit, 30 Devonshire Street, London, W1G 6PU, UK
Summary
Advances in surgical techniques and greater understanding of the anatomy of the hip now permit minimally invasive hip replacement. Benefits include shorter hospitalization and faster rehabilitation.
Introduction
Around 37,800 primary total hip replacements (THRs) are carried out in England and Wales every year. It is an extremely successful procedure, which has evolved through a series of implants and operative techniques.
There are many surgical approaches to the hip joint for THR, each having its own advantages and disadvantages. The most commonly used are the anterior and posterior approaches. Around 50% of all primary THRs are performed using the anterior or antero-lateral approach, as this is thought to give an overall superior view of the acetabulum and reduced dislocation rates compared with the posterior approach in particular. Whichever approach is used the incision tends to be relatively long, current practice is to use a single incision up to 30 cm long to approach the hip joint, with considerable cutting of muscle and other soft tissues. Trauma inevitably causes a significant inflammatory response, which delays healing.
Current surgical practice has benefited greatly from techniques which minimize surgical exposure and dissection, ranging from arthroscopy, through the wide variety of abdominal and pelvic laparoscopic procedures, thoracic surgery, to laparoscopic hernia repair. Minimally invasive surgery (MIS) of the hip joint, utilising a smaller incision with reduced tissue damage is a logical progression.
The advantages of the MIS technique arise from the reduction in trauma to the soft tissues with dissection. This reduces postoperative pain, allows greater mobility, reduces the length of hospital stay, gives a smaller scar (Fig. 1), and reduces the need for blood transfusion.
 Fig 1: Example of a mini-posterior approach scar at 6 weeks postoperatively.X-rays for every procedure.
Fig 1: Example of a mini-posterior approach scar at 6 weeks postoperatively.X-rays for every procedure.
It follows that performing the operation using a much smaller approach will cause much less trauma to the underlying tissues. There are a variety of approaches to the hip joint which are termed MIS. These range from new paths to the hip joint which have been developed that involve little or no cutting of tissues, relying instead on retraction to give a good operative field, to performing the same operation as a standard approach through either one or two smaller incisions. To facilitate good exposure through a smaller incision, there is now a wide range of specially adapted instruments available.
Some approaches require intraoperative X-ray screening to ensure correct placement of the prosthetic components as small incisions may not permit sufficient direct visualization. Techniques are being developed which rely on an electromagnetic map being made of the hip joint using small implants in the bone so that the orientation can be demonstrated without having to have exposure to harmful
Prostheses are also being introduced which cater specifically for MIS to allow easier implantation through much smaller incisions. Femoral stems in particular can be difficult to orientate and insert correctly through a small incision, and the soft tissues and skin can prevent easy insertion.
History of MIS
Despite MIS having been used as a technique since 1993 via the anterior approach, there is no clear definition of what constitutes a minimal invasive surgical procedure. Some see it as just using a smaller incision, up to 10 cm long, others as a new approach to hip surgery involving different anatomical pathways to facilitate better access through a smaller incision. Others would argue that MIS should incorporate a different technique involving less muscle cutting and therefore less soft tissue trauma, thereby enabling better recovery not just because the skin incision is small but because the trauma to the deeper soft tissues is also minimized.

Fig 2: Angled acetabular reamer compared to standard straight introducer.

Fig 3: Variety of MIS retractors.
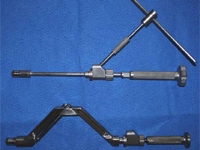
Fig 4: Angled acetabular component introducers.
The traditional approach to the hip uses instruments unsuitable for MIS, which has led to a huge number of new instruments being designed for MIS. These include specially designed retractors, somewith light attachments, angled reamers to gain access to the acetabulum for reaming without needing excessive retraction, and prosthesis introducers with longer shafts or different angles. Some examples are shown in Figs. 2-4:
Anatomical studies
The search for radically different approaches to the hip has led to re-assessment of the anatomy of the hip. These minimize tissue trauma utilising intermuscular access, where tissues are retracted and spread open rather than being cut, as well as identifying neurovascular hazards to further minimize complications. An added benefit is that with less soft tissue disruption, the risk of dislocation will be minimized.
Indications
The MIS technique is, at present, only suitable for primary THR. It may be used for cemented or uncemented prostheses.
It is contra-indicated for difficult primary THR, e.g. where there is significantly abnormal anatomy, complete hip dislocation, or where it may be necessary to perform additional procedures. A standard incision is recommended for such procedures at present.
It is not suitable for procedures such as hip resurfacing where the femoral head is preserved because exposure of the acetabulum is limited.
MIS technique is unsuitable for revision hip surgery, as this usually requires much wider exposure to remove the existing prosthesis and cement if present. There is also a higher incidence of femoral fracture during revision hip surgery which would need adequate exposure to stabilize.
Patient size may also be a limiting factor. In an obese or well muscled patient, it can be very difficult to reach the deeper structures through a small incision. The outcomes of a study into the two-incision technique found a greater number of complications if the patient’s BMI was over 30 kg/m.
Surgical technique
The approaches to the hip are broadly classified into:
- Single-incision approach
- Two-incision approach
Single incision approach
The single incision technique is currently the most commonly used MIS technique, but there is some confusion regarding correct nomenclature of the differing techniques:
- Anterior (modified Smith–Peterson)
- Anterolateral (modified Watson–Jones also referred to as the OCM technique)
- Direct lateral approach (modified Hardinge)
- Posterior approach (modified Moore)
The anterior approach
The anterior approach has many variations, mostly passing through the internervous line between the sartorius (supplied by the femoral nerve) and tensor fascia lata muscles (supplied by the superior gluteal nerve), as illustrated by Siguier et al.
The anterolateral approach
A technique developed by Heinz Rottinger (Orthopaedica Chirurgica Munich – OCM) uses an intermuscular approach anterolaterally, a modification of the Watson–Jones approach. This has been used by Bertin and Rottinger for over 300 patients. The incision starts at the anterior tubercle of the greater trochanter and extends 7 cm towards the anterior superior iliac spine. A plane is developed by blunt dissection between the tensor fascia lata posteriorly and the gluteus medius and minimus anteriorly to expose the anterior capsule which is then opened via a U-shaped capsulotomy. Using this technique no muscles or tendons need to be incised or split, which is thought to lead to better return to function of the abductor musculature. Abductor function is also preserved by avoiding the division of the anterior portions of the abductors and damage to the superior gluteal nerve is avoided. Denervation of the posterior portion of vastus lateralis is also prevented because this muscle does not need to be split.
The direct lateral approach
The mini-incision direct lateral approach, which is also sometimes confusingly referred to as the modified Hardinge approach, has been described by Ilizaliturri et al., who used standard instruments to perform the procedures in 40 patients, rather than the specialized MIS instruments used by most other surgeons for different approaches.
The greater trochanter is again the bony landmark, and an incision is made starting 2 cm proximal to the tip of the greater trochanter in its midline, extending 5-8 cm distally parallel to the long axis of the femur. The iliotibial band is incised, and the trochanteric bursa is resected. A ‘hockey stick’ incision is made through the gluteus medius muscle fibres, and gluteus minimus and rectus femoris fibres are detached from the hip capsule and greater trochanter to gain exposure to the hip capsule. After apsulotomy the hip can be dislocated in external rotation or the femoral head resected in situ with a high neck cut and then dislocated to expose the acetabulum and femur.
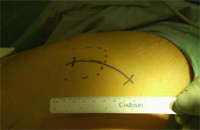 Fig 5: Posterior-mini
Fig 5: Posterior-mini
approach incision position.
In the posterior mini-incision approach the patient is positioned in the lateral decubitus position. The 6-10 cm incision is made over the posterior third of the greater trochanter in line with the femur, with one third of the incision extending proximal to the tip of the greater trochanter. The incision may be curved slightly posteriorly (Fig. 5). This gives the added flexibility of extending the incision in either direction as for a normal THR if further exposure is needed. The tensor fascia lata and gluteus maximus fascia are incised longitudinally and the muscle is split. The short external rotators are exposed and electrocautery used to detach piriformis and the short external rotators from the posterior aspect of the greater trochanter. These can be repaired at the end of the procedure with sutures passed through drill-holes made in the trochanter. After dislocating the hip the femoral head and neck are resected to expose the acetabulum. The acetabulum is reamed and the prosthesis inserted before the leg is flexed and internally rotated to deliver the proximal femur into the wound for reaming and prosthesis insertion, with the aid of further retractors to hold the proximal femur exposed.
One of the main potential risks associated with this approach in particular is the risk of sciatic neuropraxia as a result of vigorous retraction to gain a better posterior view. If the view is inadequate then it is safer to extend the incision and have a longer scar than to risk sciatic injury.
 Fig 6: Scar positions for the
Fig 6: Scar positions for the
two-incision approach.
Two-incision approach
The two-incision approach was described by Berger, and was developed and patented by the team of Dana Mears using the facilities of an anatomy laboratory to plan an approach to the hip with minimal trauma to vessels and nerves. Poor direct visualization means that intraoperative fluoroscopy is essential. The incisions are shown in Fig. 6. The patient is positioned supine on the operating table. The anterior of the two incisions is oblique, 4-6 cm in length, and made directly overlying the femoral neck, using fluoroscopy to accurately place the incision. The approach is between the tensor fascia lata muscle and the sartorius muscle superficially and then the tensor fascia lata muscle and rectus femoris muscle. No muscle fibres are cut gaining access to the capsule of the hip and incising it. The femoral head is removed in situ, enabling preparation of the acetabulum and insertion of the acetabular prosthesis. Fluoroscopy may be used for accurate reaming and placement of the prosthesis.
The more posterior/lateral incision is made as if approaching the hip to place an intramedullary nail. An awl is used to enter the femoral canal, followed by reaming and insertion of the prosthesis. Again, fluoroscopy may be used to assist in correct positioning of the reamer/rasp and prosthesis. The abductors are not cut or traumatized to any great extent during this approach.
Early complications from a multi-centre trial which started in 2001 included a 2.8% risk of proximal femoral fracture and injuries to the lateral femoral cutaneous nerve which were partial and temporary. This is acknowledged to be a more technically demanding technique than the single-incision anterior or posterior approaches, but the team developing it believe it allows much earlier discharge from hospital. However, there is currently a lack of comparative trials to back up this view.
Guided prosthesis insertion
With a mini-incision, particularly in the twoincision approach, visualization of the bony landmarks may be difficult, particularly the acetabulum. When inserting the acetabular component assisted visualization can be helpful. While most prostheses can be implanted to a reasonable degree of accuracy using just bony landmarks, navigational techniques can minimize implant misalignment, using intraoperative fiuoroscopy. This means it is less important to gain full direct visualization of the bony landmarks. Indeed, some studies suggest that the orientation of the prostheses may actually be better than direct visualization as the position is being checked fluoroscopically continuously during insertion.
The length of time fiuoroscopy is needed during a procedure diminishes as the surgeon gains experience. In this study, time fiuoroscopy was used decreased from an average of 150 s for the first case to 100 s by the tenth case.
Newer techniques, using technology which is already used in neurosurgery, where stereotactic information is provided using a three-dimensional image are becoming available. They require careful preoperative planning with scans of the pelvic anatomy, imaging equipment to process this data, and a handheld probe with various cameras around the operating theatre to judge the position of the probe in three dimensions. No intraoperative exposure to X-rays is needed, but there is a need for detailed anatomical mapping using a preoperative CT scan. It does require significant experience for the surgeon to become accustomed to this new technique.
The mini-incision technique with navigation via a posterior approach was first used in October 1998 for primary THR. Only the acetabular component was placed with navigational tools in the early series involving 33 patients. The HipNav system (Robotics Institute, Carnegie Mellon University) can be utilized for both cup and stem placement. It uses the patients’ CTscan for preoperative planning and an optical tracking system for intraoperative guidance. The surgeon selects the size and type of components and places them in an initial orientation on the pelvic and femoral models generated on the preoperative planner from the patients’ CT scan. Intraoperatively an infrared localizer determines the spatial location of markers rigidly attached to surgical tools and bony landmarks. Any acetabular component introducer handle can be equipped with tracking markers that allow active, continuous and precise tracking of the guide’s orientation relative to the pelvis. By introducing femoral tracking and navigation the system allows intraoperative control of stem placement and information regarding range of motion, offset and leg length in real time. The increased cost and exposure to radiation must be weighed against the advantages offered by computer navigation.
Sherry et al. describe a technique called the NILNAV system whereby there is no need for either a navigation system or intraoperative X-rays. They have used a CFP stem (LINK Waldemar, Germany) with various attachments to the jig and other designed instruments such as ‘‘lollipop’’ spacers to orientate the acetabular cup to the stem. Early reports on 14 patients show good results with regard to hospital discharge as well as pain and quality of life. However, this is not a universally adaptable system, and cannot be used with all types of prosthesis.
Results and benefits of MIS
Implant positioning
One of the difficulties anticipated was concern relating to accurate placement of prosthetic components. Results of 105 patients receiving uncemented implants in one study by Dorr using the posterior mini-incision approach showed good cup positioning in both anteversion (15–30o acceptable) in 92% of patients, and inclination (25–45o acceptable) in 89% of patients. Femoral placement was also good, with 90% being within 3o of neutral positioning. Wenz used a wider range of positions for the acetabulum to define normal as 35–55o inclination, and showed that acetabular positioning was good in 94% of patients. He also defined neutral alignment of the stem as being ±5o, and achieved this in all cases.
In a series of 142 patients operated on using the two-incision technique by Irving, fluoroscopy or other intraoperative imaging was not used at all. Postoperative radiographic analysis showed that the acetabular component was well positioned in 99% of these patients.
Postoperative morbidity
All patients experience pain after THR to varying degrees. Some of this pain will be a result of invasion of the bone by reaming and insertion of prostheses, cement, screws, etc. The other main source of the pain will be originating from the soft tissues. The idea is that the less soft tissues are traumatized the less this aspect of pain should be.
As well as causing the patient discomfort, pain is one of the main causes for poor mobility immediately postoperatively. By reducing their pain their mobility should be expected to be improved quite significantly. Additionally as the deeper soft tissues, and muscles in particular, have been cut much less or not at all, mobility should be improved.
Earlier mobilization should also reduce morbidity from such causes as pneumonia and basal atelectasis, deep venous thrombosis and pulmonary embolism.
The reduction in tissue trauma and the smaller skin incision, should reduce the need for blood transfusion procedures and the associated morbidity and cost. Sculco describes several small studies at his institution showing reduced blood loss (378 vs. 504 ml) in the groups of patients who had the single-incision technique as compared to a similar group having a standard incision, as well as slightly reduced surgical time and length of stay. A faster return to normal gait pattern was also seen with this group.
In a prospective study of 42 patients at the same institute having a mini-posterior approach compared to 42 patients having a standard incision, although there was no significant difference in the operative time, estimated blood loss, or length of hospital stay, there was a slightly better Harris Hip Score in the mini-incision group, and all the patients in the mini-incision group expressed greater satisfaction with their scar’s cosmetic appearance.
Earlier mobility and fewer complications results in a shorter hospital stay, with significant social and financial benefits. Mears’ study of patients having the two-incision technique showed over 90% of their patients left hospital within 24 h of surgery. A further study of 100 patients by Duwelkius et al.,4 using the two-incision method, showed 90% leaving hospital within 24 h of their THR, with the remainder leaving on the second postoperative day. However, the patients selected all weighed under 100 kg, were under 75 years old, and were less muscular than those having a standard approach hip replacement by the same surgeon.
One hundred patients in a study by Berger were operated on using the two-incision technique. As experience of the technique increased, patients were selected less according to their physical characteristics and became more representative of the usual patient group operated on in his practice. Of the last 88 patients in the study 75 (85%) were discharged home the same day as surgery.
It is to be expected that the overall rehabilitation period will be shorter as well, although there are no published studies to support this as yet.
Patients report much greater satisfaction with the appearance of a scar which is much smaller than a traditional incision. This has led to many of our patients specifically requesting a minimally invasive procedure.
Long-term outcomes
Most published data relates to the two-incision technique; there is a relative paucity of published data relating to the single-incision technique, using any of the myriad of approaches. The techniques are too new for there to be long-term follow up and/or large series to permit comparison with longterm outcome studies looking at conventional THR.
The main criticism of most published studies is that they focus on operative time, hospital stay, and radiographic analysis, rather than functional outcome and patient satisfaction. Duwelius does, however, note an average Harris Hip Score improvement from 52 points preoperatively to 90 points at 1 year (maximum 100 points).
Many surgeons who perform smaller numbers of THRs may not benefit from this technique, as more experience is needed to achieve optimum results requiring a surgeon to be performing at least 50 arthroplasties per year. This will limit the number of centres where this procedure may be carried out, and thus limit the availability of data on outcomes.
Patient selection may currently be causing bias in some studies reporting discharge times of around 24 h after the procedure. These may be younger and more active patients preoperatively, as it is clear that the older and more frail patient who already struggles with mobility due to multiple problems may not walk out of hospital so soon after having the procedure.
Future developments
Currently both the one incision and two incision approaches are being reviewed by the United Kingdom National Institute for Clinical Excellence. The lack of powerful studies and the relatively new and innovative nature of the MIS technique has meant that this review is taking some time to complete. The report on the two-incision technique is expected in late 2005, with the report on the one-incision technique expected the following year.
There have been no randomized trials, indeed some patients entered into early trials had heard of the two-incision technique and asked for it by name, and might therefore be expected to perform better as their expectations were much higher. In the same study all patients with major complications in the previous year (e.g. myocardial infarction) were excluded, as were those with three or more poorly controlled medical comorbidities.
Similarly a common theme in many of the published trials seems to be a well thought out and implemented pain management protocol which also addresses nausea and vomiting as well as dizziness. Part of this regimen involves performing surgery under an epidural, not general anaesthetic. The incidence of postoperative nausea and vomiting is thought to be reduced significantly this way, as well as ensuring adequate hydration and patients may be sedated or rendered unconscious during the procedure using agents such as propofol, rather than any anaesthetic agents.
Patients in one study would attend classes preoperatively and be taught by a specialist nurse what to expect from the operation, immediate postoperative phase and recovery process. They were also told that they would be able to walk independently on the day of their operation. This was reinforced by intensive physiotherapy and occupational therapy, which were started as early as 5 h postoperatively.
Hence if patients’ expectations of their operation are that they will have a tremendous improvement in function immediately postoperatively, compared to the general perception of having severe pain and immobility after a THR, then they are more likely to have a better immediate outcome. Thus, what proportion of this rapid recovery is due to careful preoperative preparation of patients, patient selection, postoperative pain and nausea regimens, and early intensive physiotherapy, and how much is due entirely to the operative technique remain unclear.
Therefore large studies are needed with traditional techniques being compared directly with MIS approaches. This must include patient selection, preoperative explanation and counselling, anaesthetic techniques, postoperative analgesic and physiotherapy regimens, as well as functional and radiological analysis in the long term and not just concentrating on the operative data. Only then will the true value of the MIS technique be known.

No Comments